Listen Instead of Reading
If you enjoy listening, you can subscribe to the audio version on Spotify, Apple Podcasts, and Audible so you don’t even have to look at the email 😊
4 THOUGHTS
1. The Most Helpful Breathing Tip I’ve Found (it’s embarrassingly cliché & simple)
Don’t take ten breaths. Take one breath, ten times.
Don’t do 5 minutes of breathing. Consciously take one breath, over and over, until your 5-minute timer goes off.
Sounds silly, but it works 👏
2. How to Build a Stronger Mind
In Peak Mind, Dr. Jha describes a “mindfulness push-up” as the following:
You shine your attention on your breath.
Your mind wanders, and you notice it.
You redirect your mind to your breath.
“This is what we might call the ‘push-up’ of a mindfulness breathing exercise.”
I love this analogy because it conveys the most crucial aspect of mindfulness: Just like repeated physical push-ups make our muscles stronger, repeated “mindfulness push-ups” make our minds stronger.
Meaning we need our minds to wander so we can notice it and come back to the breath. It’s how our minds get stronger.
3. Breathing Must Be Practiced Not Just in Solitude
“Spirituality must be practiced not just in solitude but also among people. Open up to people around you and feel connected. This is the true challenge of spiritual practice.”
- Haemin Sunim, The Things You Can See Only When You Slow Down
The same is true for our breathing (or any contemplative) practice. It must be performed not only in solitude, but in real life:
How we do (or do not) reply to comments on social media is our practice.
How we do (or do not) reply to emails that provoke us is our practice.
How we do (or do not) interact with friends & family is our practice.
And on and on for every aspect of our lives…
So, this is the true challenge: To use our favorite contemplative practice to fundamentally change who we are and how we interact with the world for the better.
4. Two Ways to Keep Your Practice Interesting
Switch up your routine or exercises every 15-30 days to continuously create novelty.
Cultivate mindfulness so the same old boring exercises continuously create novelty.
P.S. There’s no right or wrong, and you can use both approaches simultaneously 😊
1 Quote
“Practicing to walk and breathe mindfully helps you dwell more in the real world, so you can get in touch with the wonders of life in the present moment, and nourish and heal your body and mind.””
1 Answer
Category: Breathing Basics
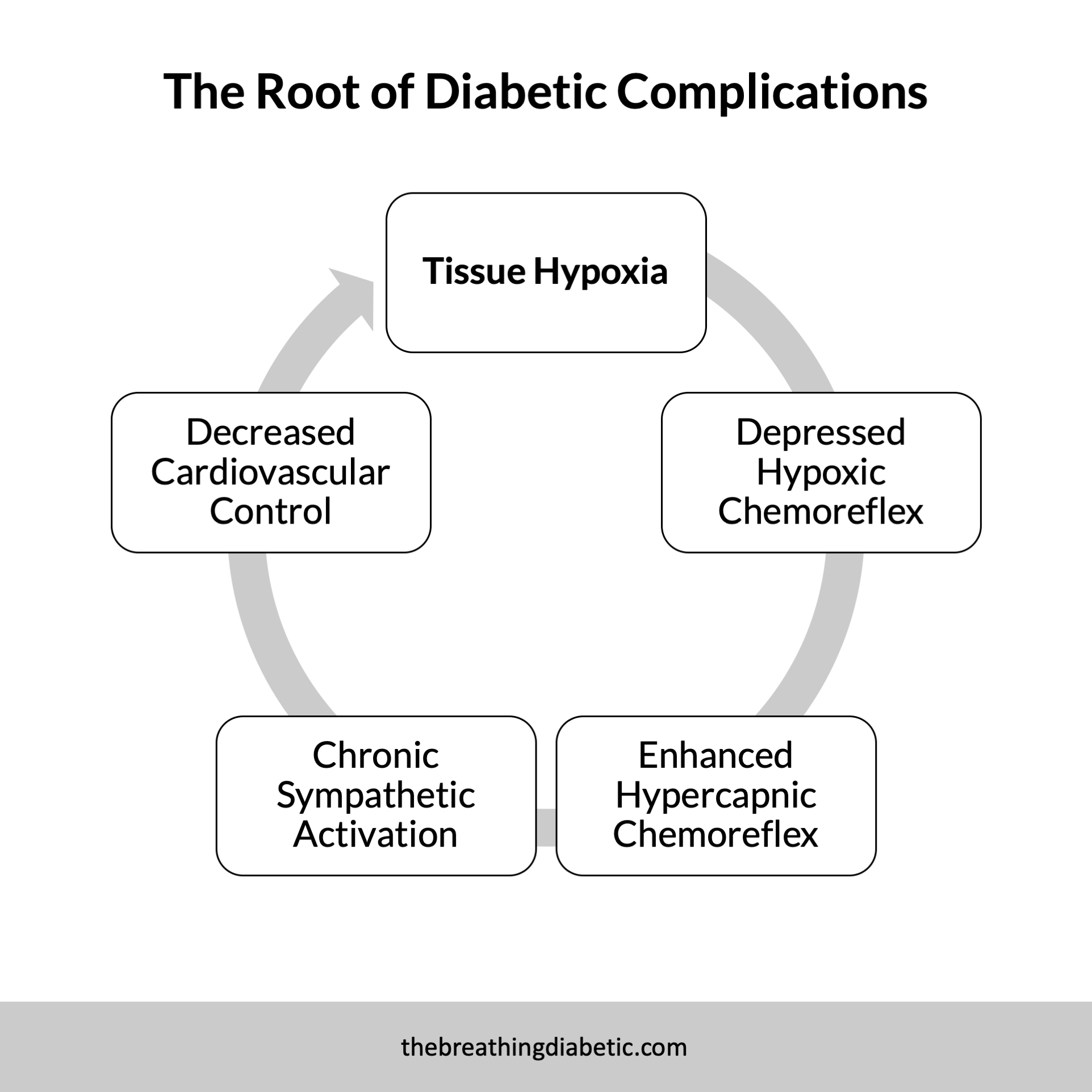
Answer: The way your breathing responds to high carbon dioxide or low oxygen is generally referred to as this.
…
(Cue the Jeopardy! music.)
…
Question: What is chemoreflex sensitivity?
In good breath,
Nick Heath, T1D, PhD
“Breathing is the compound interest of health & wellness.”
P.S. Every single morning
* An asterisk by a quote indicates that I listened to this book on Audible. Therefore, the quotation might not be correct, but is my best attempt at reproducing the punctuation based on the narrator’s pace, tone, and pauses.