Wim Hof vs. Slow Breathing: The Famous Endotoxin Experiment
I’ve called the Wim Hof endotoxin study the “4-minute mile” of breathing. It showed, scientifically, that conscious control of our immune response is possible with the breath and mind.
However, I did not know that four years before the Wim Hof Method (WHM) study, a paper was published looking at the effects of slow breathing on endotoxin exposure. There are significant differences between the studies, but this is about as close an accidental comparison as you can get in the “breathing world.”
In this short post, I break down the two studies and their general conclusions. Spoiler alert (but perhaps not surprising): The WHM is much more effective than slow breathing for fighting off acute inflammation.
A Very Basic Overview of the Concept
Exposure to endotoxin is a controlled method of activating and studying the body’s immune and inflammatory responses. There are generalized responses that have been documented in a relatively large set of participants. Thus, it provides an excellent way of analyzing how different training approaches and medications can influence the body’s inflammatory response.
The Wim Hof Study
Twelve participants learned the full WHM (breathing, cold exposure, and third-eye meditation) from Wim himself and a few other WHM instructors. They trained with them for four days and were advised to practice independently at home leading up to the study (generally 2-3 hours a day). Before the study, Wim led them through one more session, and Wim was also present throughout the endotoxin experiment. This is important because Wim is charismatic; he undoubtedly provided a placebo effect.
In fact, a separate study published in 2016 found that after training with Wim, the participants’ “outcome expectancies” rose significantly (meaning they expected the WHM to help them fight off the endotoxin). The authors found that this correlated significantly (correlation is not causation) with the reductions in subjective symptoms during the endotoxin exposure. However, a more recent 2020 study (which, from what I can find, is still in preprints and hasn’t undergone peer-review) indicated that very similar results can be obtained even without Wim doing the personal training. So, maybe Wim played a role, maybe not.
Another twelve participants were the control group, performing no additional training before exposure to the endotoxin.
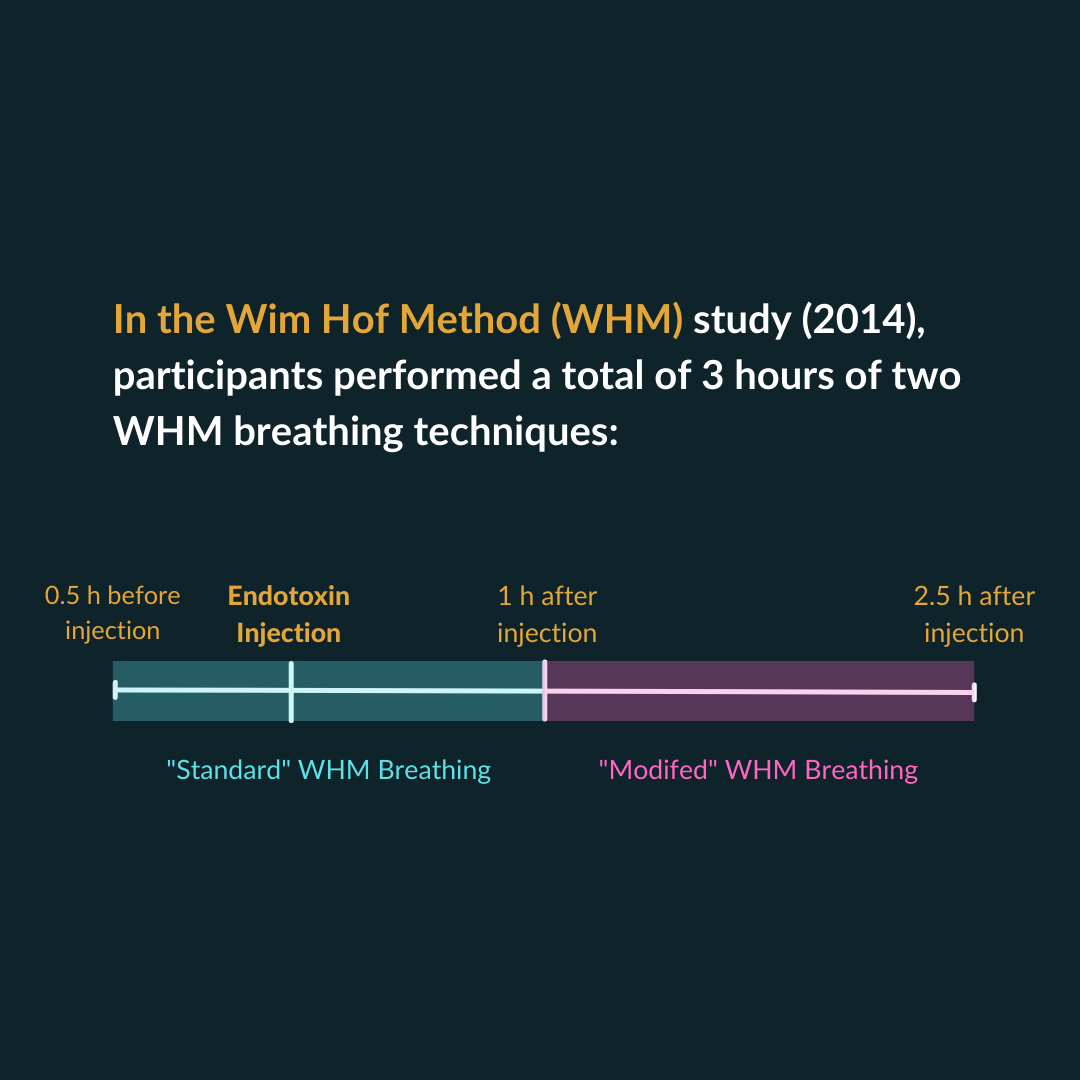
What Did the WHM Group Do During the Experiment?
Thirty minutes before endotoxin exposure, the WHM group started the standard WHM breathing protocol. They were exposed and continued this breathing for an hour (so 1.5 hours of the standard WHM). Then, from hour 1 to hour 2.5 (another 1.5 hours), they performed basically the same thing, but instead of the regular WHM breathing, they did ~30 big breaths, held and tightened all of their muscles for 10 seconds, and then let go (so no drop in oxygen saturation with this technique).
Overall, the participants performed approximately 3 hours of continuous breathing split between these two techniques.
What happened?
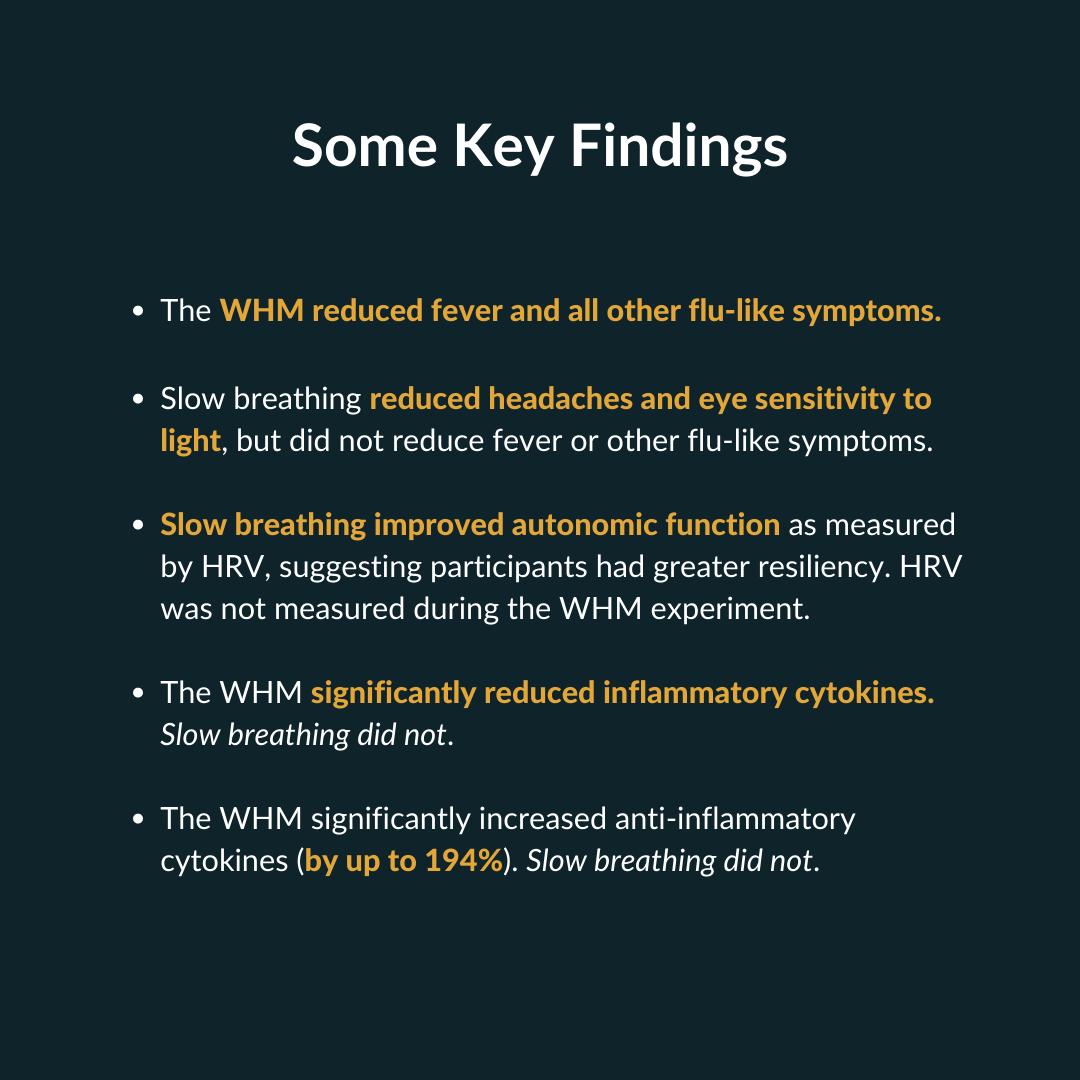
The participants significantly suppressed inflammatory cytokines and increased anti-inflammatory cytokines (a 194% increase in one anti-inflammatory cytokine). They had huge increases in adrenaline, which correlated with these changes in cytokines. They also reduced their fever and significantly reduced the number of symptoms they felt (at the peak, their symptom score reduced by ~56% compared to the control group). However, as mentioned earlier, a separate study found that reductions in symptoms were significantly correlated with how much they expected the WHM to work. In any case, correlation is not causation, and I’m not sure if it really matters—either way, it worked, which was the test of this experiment.
These results were groundbreaking, upending most of what is known about the innate immune and inflammatory responses. These results put the WHM on the map scientifically.
The Slow Breathing Study
Six participants learned to breathe at their resonant frequency. They underwent four 1-hour HRVB sessions leading up to the endotoxin exposure. The first two were a few days before the exposure, the third was the night before, and the fourth was the morning before exposure. After the first session, the participants were told to practice their paced breathing at home for 20 min, 2x a day (recall that the WHM participants were practicing the method ~2-3 hours a day before the endotoxin experiment).
A major difference with the WHM study is that, in the slow breathing experiment, the control group (n=5) underwent this exact same breathing procedure, except they were simply taught to breathe at 15 breaths per minute, which is close to a spontaneous breathing rate. This is super important because they were still practicing a controlled breathing technique. In contrast, in the WHM experiment, the control group underwent no training.
We know that conscious control of our breath, even if done at a relatively fast pace, can still affect the autonomic nervous system. For example, one study found that controlled breathing at 12 breaths per minute reduced sympathetic activity. Thus, this is a significant difference from the WHM study because the control group was not completely inactive. (Technically, this is a better-designed experiment since we have a placebo-controlled group. But, in this case, I personally wish the control group would have been completely inactive for better comparison with the WHM study…I digress…)
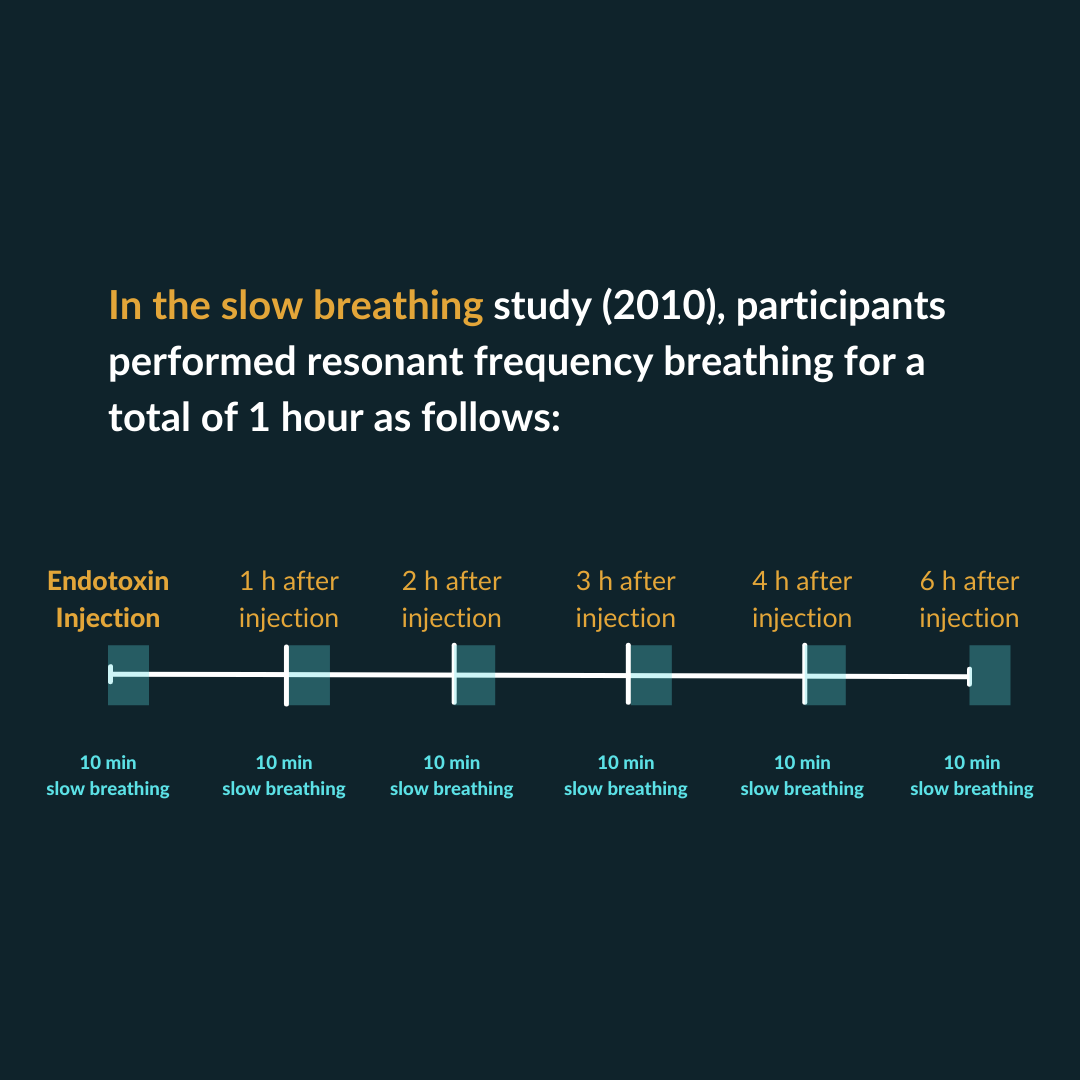
What Did the Slow Breathing Group Do during the Experiment?
This is where it gets very different from the WHM study. The participants performed 10 minutes of slow breathing every hour for 4 hours, then once more at hour 6. So, it looked like this:
10 minutes of slow breathing when receiving the endotoxin (hour 0)
10 minutes at hour 1
10 minutes at hour 2
10 minutes at hour 3
10 minutes at hour 4
10 minutes at hour 6
Thus, they performed a total of 1 hour of slow breathing over 6 hours after exposure to endotoxin. This is significantly different from the WHM endotoxin approach, where the participants practiced the method for 3 hours straight (including thirty minutes before to prime their nervous systems). Who knows what might have happened if they performed the HRV breathing for the duration of the experiment rather than in 10-minute chunks? Unfortunately, we have to take what we can get in the breathing science world 😊
Also, note again that the control group did the same protocol, except they breathed at 15 breaths per minute.
What Happened?
Notably, the participants dampened the autonomic response to the endotoxin. For example, it’s documented that exposure to endotoxin significantly reduces HRV (and thus your resiliency). In the slow breathing group, the reduction was not as great, even at rest (that is, their HRV was still higher even when they weren’t practicing slow breathing). This would indicate they were more resilient to fight off the endotoxin.
The slow breathing group also suffered fewer headaches and was less sensitive to light (two common side effects of endotoxin exposure). However, other symptoms (nausea, muscle aches, chills) remained basically the same, and they did not reduce their fevers like the WHM group did.
Finally, the authors state that there were no significant differences in inflammatory markers. They did not show the data, so there’s no way of knowing if there was a non-significant effect. So, maybe it helped a little bit? Maybe it hurt a little bit? We can’t say for sure.
Either way, the WHM showed significant (and quite dramatic) positive changes in inflammatory markers. In contrast, the slow breathing group showed no significant differences.
The Take-Home Messages
This was not a perfectly-designed direct comparison of the Wim Hof Method vs. Slow Breathing for the endotoxin study. However, given that the studies were published four years apart, it’s about as close a random chance as we could ask for in the breathing science community.
And based on the limited results, the Wim Hof Method was decidedly more effective than slow breathing at reducing inflammation and fighting off the flu-like symptoms of endotoxin. Slow breathing did help some, just not to the extent that WHM did.
Some Concluding Thoughts
Slow breathing has never been thought of as a way to acutely fight off infection. Instead, it’s generally considered an everyday practice to reduce stress, increase vagal tone, and enhance overall resiliency. So, it would be interesting to see the results in participants who practiced slow breathing for a longer period (say 3+ months) before the exposure compared to completely non-trained individuals.
Moreover, the point of all this “breathwork” stuff is to have different tools for different situations. So, what might be even more fascinating is to look at the daily practice of slow breathing for increased resiliency, followed by the WHM for the endotoxin experiment (mixed breathing artist style). Maybe we’d get the best of both worlds?
Finally, if you’re a true breathing nerd, I highly recommend you check out the more recent 2020 WHM endotoxin study that’s still in preprints. It’s too deep to go into here, but it’s packed with exciting findings on the WHM.
KEY REFERENCES
The Slow Breathing Endotoxin Study
Lehrer P, Karavidas MK, Lu SE, Coyle SM, Oikawa LO, Macor M, Calvano SE, Lowry SF. Voluntarily produced increases in heart rate variability modulate autonomic effects of endotoxin induced systemic inflammation: an exploratory study. Appl Psychophysiol Biofeedback. 2010 Dec;35(4):303-15. doi: 10.1007/s10484-010-9139-5. PMID: 20635134.
The Wim Hof Endotoxin Study
Kox M, van Eijk LT, Zwaag J, van den Wildenberg J, Sweep FC, van der Hoeven JG, Pickkers P. Voluntary activation of the sympathetic nervous system and attenuation of the innate immune response in humans. Proc Natl Acad Sci U S A. 2014 May 20;111(20):7379-84. doi: 10.1073/pnas.1322174111. Epub 2014 May 5. PMID: 24799686; PMCID: PMC4034215.
The 2020 WHM Study Still in Preprints
Zwaag, Jelle & Naaktgeboren, Rick & Herwaarden, Antonius & Pickkers, Peter & Kox, Matthijs. (2020). The combination of cold exposure training and a breathing exercise attenuates the inflammatory response in humans. 10.21203/rs.2.20192/v1.